Tuberculosis is caused by mycobacterium tuberculosis. It involves type 4 hypersensitivity causing caseous necrosis. When a clinical question comes where tuberculosis is one of the options, pointers towards tuberculosis can be symptoms, chest X-ray, sputum microscopy & culture. Let’s discuss how to arrive at the diagnosis of TB.
Patient with any age having long-standing fever (especially, evening-rise fever), weight-loss (loss of more than 5% of the highest weight recorded in the past three months), and cough should raise the suspicion of TB. Loss of appetite & fatigue are other symptoms. Alcoholism, overcrowding, malnutrition & HIV are the frequent associations of tuberculosis. In pediatric age group, H/o contact with a TB case is extremely important. MCQ may give description of a case & chest X-ray (CXR) of the patient. The CXR in MCQs most offenly shows any of the following manifestations:
Ghon’s complex: Active tuberculosis disease has been classified as either primary or post-primary tuberculosis. Primary TB is common in the pediatric age group & manifests as Ghon’s complex, usually affecting the middle and lower lobes. When the bacillus enters the lung, a small patch of caseous bronchopneumonia develops and later encapsulates. This is the primary focus called as Ghon focus. The (a) primary focus, (b) lymphangitis (inflammation of lymph vessels connecting primary focus to hilar lymph nodes), and (c) perihilar lymphadenitis is collectively called as Ghon’s complex or primary complex of Ranke.
- Cavitary TB: Upper lobe cavitary tuberculosis is the hallmark of post-primary TB and this appears in about half of the patients. Post-primary TB is common in adults; this is mainly located in the apical and posterior segments of the upper lobes. There can be various non-infectious differentials for cavitary lesions in the lungs like pulmonary embolism, CA Lung, Wegener’s Granulomatosis & sarcoidosis. Among infectious causes Klebsiella pneumoniae is a common cause of severe, necrotizing pneumonia frequently complicated by lung abscess, which generally appears as one or more cavities. Staphylococcus aureus is another important cause of cavitary pneumonia. But TB stands the number 1 diagnosis for cavitary lesions in CXR in Indian scenario. Although, TB presents in various other ways in CXRs, above 2 forms are the most important NEXT or NEET-PG point of view.
Culture media for tubercular bacilli: 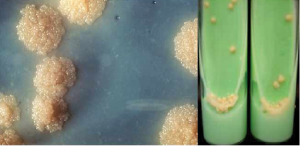
Tuberculin test (Mantoux test):
Tuberculin i.e. purified protein derivative (PPD) is injected intradermally. Induration (NOT erythema) ≥ 10 mm is considered as positive test. It is not used for the diagnosis of TB.
Positive test indicates hypersensitivity (type 4) to tuberculin protein which may be due to:
- Active infection
- Subclinical infection
- Past infection
- BCG vaccination.
Government of India has started Revised National TB Control Program (RNTCP). In 2020 the RNTCP was renamed the National Treatment Elimination Program (NTEP) to emphasize the aim to eliminate TB in India by 2025.
Adverse effects of anti-tubercular drugs is an extremely favorite topic in NEET-PG & FMGE. Numerous clinical scenarios can be formed on these side-effects. Following table will help you immensely to deal with such MCQs.
| Drug | Adverse effects |
| Isoniazid | Peripheral neuropathy, hepatitis |
| Rifampicin | Immuno-allergic reactions, GI disturbances, hepatitis, thrombocytopenic purpura |
| Ethambutol | optic neuropathy (retrobulbar neuritis) |
| Pyrazinamide | Hepatitis, hyperuricemia affecting joints, GI disturbances |
| Streptomycin | Renal and cochleo-vestibular toxicity |
INH Prophylaxis: If the child < 6 years does not have active TB, isoniazid (INH) is recommended at the dose of 10 mg/kg daily for a duration of 6 months, if such a child is in close contact of a case of TB. E.g. if mother has TB, her child of less than 6 years age should be offered INH prophylaxis if that child doesn’t have TB.
Happy studying for NEXT exam!
– Dr. Vaishali Giribhttanavar


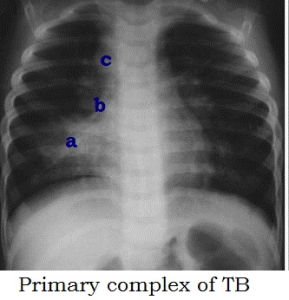 Ghon’s complex: Active tuberculosis disease has been classified as either primary or post-primary tuberculosis. Primary TB is common in the pediatric age group & manifests as Ghon’s complex, usually affecting the middle and lower lobes. When the bacillus enters the lung, a small patch of caseous bronchopneumonia develops and later encapsulates. This is the primary focus called as Ghon focus. The (a) primary focus, (b) lymphangitis (inflammation of lymph vessels connecting primary focus to hilar lymph nodes), and (c) perihilar lymphadenitis is collectively called as Ghon’s complex or primary complex of Ranke.
Ghon’s complex: Active tuberculosis disease has been classified as either primary or post-primary tuberculosis. Primary TB is common in the pediatric age group & manifests as Ghon’s complex, usually affecting the middle and lower lobes. When the bacillus enters the lung, a small patch of caseous bronchopneumonia develops and later encapsulates. This is the primary focus called as Ghon focus. The (a) primary focus, (b) lymphangitis (inflammation of lymph vessels connecting primary focus to hilar lymph nodes), and (c) perihilar lymphadenitis is collectively called as Ghon’s complex or primary complex of Ranke.

